
Chief Growth Officer
Penny Reed is the Chief Growth Officer at eAssist Dental Solutions and author of Growing Your Dental Business. With over 30 years of experience as a dental business coach and speaker, Penny was named a Leader in Dental Consulting by Dentistry Today from 2007 to present. A former IT manager at Walmart turned dental practice leader, she is a certified Behavioral Consultant and former Dale Carnegie Trainer. At eAssist—the nation’s leader in outsourced dental billing—she serves on the executive team and speaks nationally on team coachability, revenue cycle management, and practice growth. Penny is a member of the Speaking and Consulting Network, the American Association of Dental Office Management, faculty at the Nash Institute, and an advisor for the University of Tennessee’s Digital Marketing certification program.
Dr. It’s Time To Give Yourself A Raise
Henry Schein recently launched the Give Yourself A Raise tour. This revenue cycle management boot camp provides dentists with the training and tools they need to increase their profits. Featuring eAssist Dental Solutions, Unitas PPO Solutions, and Practice Booster, this event provides dentists the unique opportunity to learn from the industry’s leading insurance experts. These events range from half-day to full-day sessions with corresponding CE credits available. Check out the upcoming event days, locations, and registration links below (updated monthly!):
| DATE | LOCATION | REGISTRATION LINK |
| 2024 dates coming soon! | Check back here for more info | Registration link to come |
In the meantime, you can get your very own “sneak peek” of the event by reading this blog post!
What does it mean to give yourself a raise?
As the dentist, you get a raise when your practice’s profits increase. There are two simple ways to make more profit and give yourself a raise: increase revenue or decrease expenses. The Give Yourself a Raise Tour focuses on the top strategies to boost revenue.
More specifically, we cover the 3 C’s of revenue cycle management: contracting, coding, and collecting. Contracting refers to PPO network contract negotiations and optimization to increase your fee schedules. Coding is using the correct dental codes to maximize insurance reimbursements. Collecting refers to increasing the money obtained through both insurance and patient billing procedures.
Contracting
Network participation doesn’t necessarily lead to increased patient acquisition. The main value that comes from network participation is increased treatment acceptance. Obviously, treatment acceptance is vital to the practice, which means you have a great reason to participate in PPO networks. So, now you need to determine how to participate in a way that maximizes your revenue.
An effective revenue strategy should result in a set of “target fees.” These fees will provide the practice with a revenue stream that allows the practice to provide high quality care to patients, while at the same time providing a fair income to the provider.
Contract Negotiation
Once you know your target fees, you should negotiate all insurance PPO fees schedules and contract items in order to implement your revenue strategy. This is not a one-time task. You must continue to negotiate code by code on an ongoing basis with the insurance companies in order to represent the dental community and resist timetables controlled by the insurance industry.
Participation Optimization
Another key to achieving your target fees is through participation optimization. The goal with optimization is to enable your practice to see the maximum number of patients at the highest reimbursement levels under the fewest number of contracts. Establishing the correct mix of PPO participation is critical to increase reimbursement levels, reduce insurance adjustments, increase exposure to new patient flow, and decrease patient loss from out-of-network plan provisions. When optimizing your network, aim for participation diversification. This is helpful to reduce exposure to third-party leverage.
Credentialing & Compliance
Proper credentialing is extremely important in effective PPO cash flow management. The insurance industry utilizes the credentialing process to reduce reimbursements and delay payments, making the proper management of the process critical to the practice.
Managing and negotiating PPO contracts can be complex to say the least. If you’re looking for an expert to handle this critical function for you, Unitas PPO Solutions can help. Unittas analyzes your UCRs and production, verifies PPO participation per doctor per location, analyzes participation and fee schedules, negotiates with direct contracts, and optimizes all PPOs under the most profitable participation. They also provide ongoing support by auditing EOBs to ensure negotiations and optimizations fall into place, monitoring your PPO participation, and negotiating and optimizing long-term as new opportunities arise.
Coding
One simple way to boost your revenue is to ensure your team is coding correctly. Understanding how to properly report dental procedures, and providing the documentation required by payers, is essential to receiving payment for dental services. Claims are often denied due to incorrect CDT codes, missing documentation & attachments, or severe delays in submission (i.e., timely filing).
Correct coding often results in higher revenue, as practices obtain reimbursements that were once unpaid because of misunderstanding or misreported codes.
— Dr. Charles Blair
The number 1 dental coding rule is to code and report “what you do.” Additionally, you must remember that codes are not specialty specific, and codes are updated annually. Over the last 3 years alone, there have been 160 changes to ADA CDT codes. Without an up-to-date coding resource, you risk having claims denied unnecessarily.
How do you find coding resources that best suit your office’s needs?
Choosing the right coding resources for your dental practice is crucial in order to accurately document dental procedures and billing. The American Dental Association (ADA) Current Dental Terminology (CDT) coding guides and Practice Booster’s “Coding with Confidence” are considered top-tier resources in this field. They are developed by expert dental professionals to ensure the correct coding of dental procedures. To ensure that these resources best suit your dental practice’s needs, consider the following:
- Understand Your Needs: Consider your office’s specific needs. Do you need a comprehensive resource for all procedures, or are there only certain areas where you need more help? Do you want a hard copy guide, an online resource, or both?
- Training: Do you and your team need training to understand these codes better? If so, consider purchasing the resources that offer extensive educational support like webinars, online training, and more.
- Budget: Consider the costs of these resources and how they fit into your practice’s budget.
- Up-To-Date Information: Dental codes change over time, so make sure to get the latest version of any resource you choose, and stay updated on changes and revisions in the future.
Coding Resource Ex – practicebooster.com

Practice Booster is known for its product “Coding with Confidence,” which is designed to optimize dental coding and maximize reimbursement while ensuring compliance. The tool offers insights into how to use codes correctly and includes many real-life examples. To utilize this tool, you can visit the Practice Booster website and purchase the “Coding with Confidence” manual. Practice Booster also offers online training, webinars, and other educational resources to help you make the most out of their tool.
In short, CDT codes are changed and updated frequently. To maximize your reimbursement and give yourself a raise, you need updated coding resources to ensure your team is using the correct codes.
Collecting
The ideal net collection ratio for a dental practice should be at least 98% each month, but 100% is even better. Unfortunately, the average dentist is collecting only 91% each month. That extra 9% adds up in terms of missed revenue. For example, an office with annual net production of $800,000 is missing out on over $2 MILLION over 30 years.
How can you improve your collection ratio?
Start by identifying the cracks in your revenue cycle management pipeline. This pipeline begins the moment the patient is scheduled and includes all steps until the balance is collected from insurance and the patient. Take a look at the pipeline below and identify the top 2-3 areas your team could improve.
REVENUE CYCLE MANAGEMENT PIPELINE
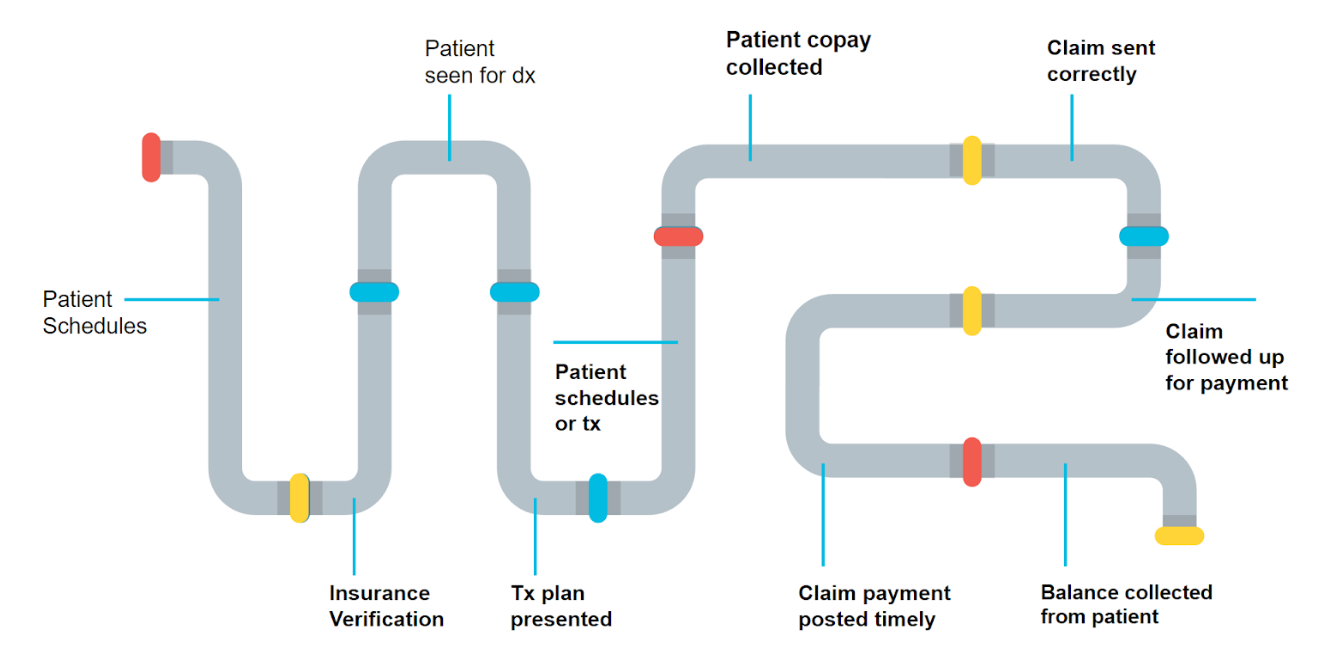
- Develop a Pre-appointment Readiness Plan
- Attach the correct CDT code to the service provided
- Obtain all necessary clinical documentation
- Send clean primary and secondary claims
- Support the appeal process (when applicable)
The hidden costs of insurance management
The average time on hold with an insurance company is 43 minutes PER CLAIM. This means you not only need team members with time, experience, and dedication, you need a compensation model based on collections versus hourly pay. eAssist Dental Solutions can help. Your in-office team can focus on patient care, patient experience, and growing the practice while your eAssist team handles insurance claim processing. Through eAssist, you can outsource dental billing, insurance verification, patient billing, accounting and bookkeeping, and more.
Conclusion
In conclusion, giving yourself a raise requires a strategic approach to practice revenue management that focuses on boosting revenue and controlling expenses. Mastering the 3 C’s of revenue cycle management—contracting, coding, and collecting—plays a crucial role in enhancing revenue. By effectively negotiating contracts, optimizing dental codes, and improving billing procedures, you can increase your profit margins and ultimately give yourself a much-deserved raise. To learn the top strategies for contracting, coding, and collecting, register for a Give Yourself a Raise event near you!
Spotlight
The 7 Deadly Sins of Dental Claims Denials
Learn how to avoid the most common claim mistakes and get paid faster.
Download eBook

Dental Insurance Billing Done for You
Discover how eAssist helps practices simplify billing and boost collections.
See How It Works

Talk to a Dental Billing Specialist
Not sure where to start with medical billing? Let’s talk.
Book a Consultation